What Did Jules Do In The Mental Hospital? Exploring Support For Dissociative Identity Disorder
Many people wonder about the journey someone like Jules might experience when receiving care in a mental health setting, especially if they are dealing with conditions that are often misunderstood. It's a question that brings up curiosity about what really happens behind those doors, and how people find their way to a better place. Today, we are going to look at the kind of help and support someone with dissociative identity disorder (DID) could find in such a place, using a hypothetical person like Jules as our example.
This discussion aims to shed some light on what treatment for dissociative identity disorder often involves. We want to show how a person might begin to feel more at peace and put together the pieces of their life. It's about understanding the path to well-being for individuals who live with separate parts of themselves, a condition that is, in fact, rather rare.
Our goal is to give you a clearer picture of the support available. We hope to offer a sense of solace for those who are personally dealing with dissociative conditions, and also for friends and family members who are standing by someone with this kind of mental health challenge. So, let's explore what a stay might look like.
Table of Contents
- Understanding Dissociative Identity Disorder
- The Purpose of a Mental Health Stay for DID
- Initial Steps and Assessment
- Talk Therapy: The Main Treatment
- Group Sessions and Community Support
- Learning Coping Skills
- Supporting Friends and Family
- Addressing Misconceptions
- Life After the Hospital
- Frequently Asked Questions
- Finding Peace and Progress
Understanding Dissociative Identity Disorder
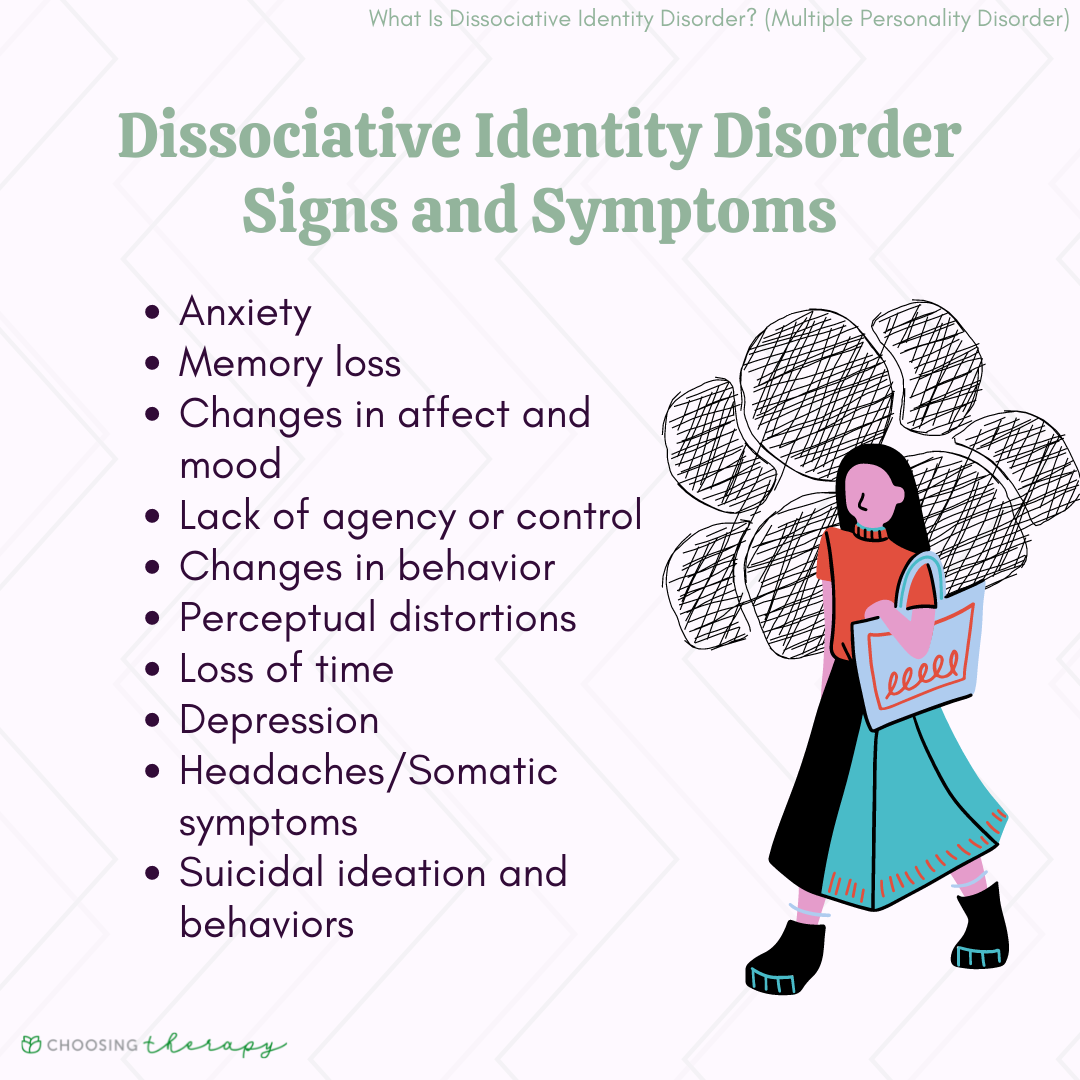
Dissociative identity disorder, often called DID, is a mental health condition where a person has two or more separate personalities. These distinct parts, or "alters," can take control of behavior at different times. It's a condition that has been known by other names, too, like multiple personality disorder, which you may have heard before, or split personality.
The presence of these distinct identity states is what characterizes DID. These different parts might have their own memories, ways of acting, and even different ways of seeing the world. It's a disturbance of identity, really, where two or more separate and relatively lasting identities are present in an individual, and they take control alternately, you know.
DID is a rather rare mental health condition. It involves a disruption of identity and reality for the person experiencing it. Individuals with DID will show two or more distinct identities, and it's a condition that is very often misunderstood. It gets portrayed incorrectly in popular media, which can make it harder for people to grasp what it truly is.
The Purpose of a Mental Health Stay for DID
When someone like Jules enters a mental health facility, the purpose is not just about keeping them safe. It is also about giving them a structured and supportive place to begin their healing. For someone with dissociative identity disorder, a hospital setting can offer a safe haven, a place where they can start to make sense of their experiences without the pressures of daily life.
This kind of environment provides a chance for intensive, focused care. It allows mental health professionals to observe and understand the person's needs in a way that might not be possible in outpatient settings. The aim is to stabilize the individual and begin the important work of therapy, so they can feel more like themselves.
So, for Jules, a stay might mean a break from everyday stressors. It's a place where they can focus completely on their mental well-being. This can be especially helpful if they are having a hard time managing their different identity states on their own, or if their daily life has become too much to handle, you see.
Initial Steps and Assessment
Upon entering a mental health hospital, the first step for someone like Jules would be a thorough assessment. This means a team of professionals would spend time getting to know them. They would try to understand their history, their symptoms, and how their dissociative identity disorder affects their life, actually.
This assessment helps the team create a personalized plan of care. They look at the distinct identity states, how they show up, and what triggers might cause shifts between them. It's about gathering all the necessary information to provide the most helpful support possible, which is really important.
They might ask about past experiences, about any trauma, because DID often has roots in severe, repeated trauma during childhood. Understanding these past events is a very big part of putting together the puzzle of the person's present condition. This initial phase is crucial for building trust and setting the stage for recovery, you know.
Talk Therapy: The Main Treatment
The main treatment for dissociative identity disorder is talk therapy, also known as psychotherapy. For Jules, this would mean spending a good deal of time with a therapist. These sessions are a safe space to explore thoughts, feelings, and experiences, so they can start to put things in order.
The therapy aims to help the different identity states communicate and work together. It's about helping the person build a sense of wholeness, rather than having separate parts that control their behavior at different times. This process can be long and challenging, but it is also very rewarding, in a way.
A therapist helps the person understand their alters. They also help them learn ways to manage switches between these states. This involves gentle exploration of difficult memories and working towards integration, or at least cooperation, among the different parts of the self. It's a gradual process that requires a lot of patience and trust, apparently.
The therapist might use various techniques within talk therapy. These can help Jules process past events and develop new coping strategies. The goal is to lessen the impact of the dissociative symptoms and help the person live a more unified life. This takes time, but it really makes a difference.
Through consistent sessions, Jules would likely gain a better grasp of their condition. They would learn to recognize the signs of shifts in identity and how to respond in a way that helps them stay present. It's about building internal resources and strength, you see, so they can manage their daily life outside the hospital setting.
The therapeutic relationship itself is a very important tool. Having a consistent, trustworthy person to talk to can provide a sense of stability. This is especially true for someone whose internal world might feel chaotic. It creates a foundation for healing, which is quite vital.
Group Sessions and Community Support
Besides individual talk therapy, Jules would likely participate in group sessions. These groups offer a chance to connect with others who are also working through their own mental health journeys. It can be incredibly helpful to know you are not alone, you know, and that others share similar experiences.
In these groups, people can share their stories and offer support to one another. It's a place to practice new social skills and learn from the experiences of peers. This community aspect can be a very powerful part of the healing process, giving people a sense of belonging and mutual aid.
These sessions might focus on various topics, like managing emotions, dealing with stress, or building healthier relationships. The group setting provides a safe space to try out new ways of being and interacting. It helps build confidence for when they return to their daily lives, too, it's almost like a practice run.
For someone with DID, group therapy can also help with feeling more connected to others. It can reduce feelings of isolation that often come with the condition. Hearing others talk about their struggles and triumphs can be really inspiring and provide a sense of shared purpose, you know.
It's about creating a supportive network. This network can extend beyond the hospital walls once a person leaves. These connections are pretty important for long-term well-being and continuing to grow outside of a structured environment, so they can keep making progress.
Learning Coping Skills
A big part of what Jules would do in the mental hospital is learn new ways to cope with their feelings and triggers. This goes beyond just talking about problems; it involves practical tools they can use every day. These skills help manage distress and maintain stability, as a matter of fact.
They might learn about grounding techniques. These are simple actions that help a person stay present in the moment when they feel overwhelmed or disconnected. Things like focusing on their breath, touching a textured object, or naming five things they can see, hear, or feel can be very helpful.
Mindfulness practices could also be introduced. This involves paying attention to the present moment without judgment. It helps to observe thoughts and feelings without getting caught up in them. This can be a powerful way to reduce anxiety and increase self-awareness, you know.
Distraction techniques are another tool in the coping kit. When intense emotions or difficult memories arise, having healthy ways to redirect attention can be very useful. This might include engaging in hobbies, listening to music, or doing something creative, so they can shift their focus.
Problem-solving skills are also taught. This helps people identify challenges and come up with practical solutions, rather than feeling stuck. It empowers them to take control of situations and feel more capable in their own lives, which is a pretty big step.
The hospital environment provides a safe place to practice these skills. The staff can offer immediate feedback and support as Jules tries out new ways of responding to their internal experiences. This hands-on learning is truly valuable, you see, for building lasting habits.
Supporting Friends and Family
The journey of someone with DID also involves their loved ones. A mental health facility often provides support and education for friends and family members. This helps them understand the condition better and learn how to be a source of strength, in a way.
Family sessions might be part of the treatment plan. These sessions help open up lines of communication and address any misunderstandings. They can also teach family members how to recognize the signs of distress and how to offer appropriate support, which is quite important.
Educating loved ones is a big part of creating a supportive environment for when Jules returns home. They learn that DID is a real medical condition, not just someone "making things up." This knowledge can help reduce stigma and build stronger, more understanding relationships, you know.
For those supporting someone with DID, it can be a lot to take in. The hospital staff can offer resources and guidance. They can help them cope with their own feelings about the situation, and learn how to best help their loved one without feeling overwhelmed, as a matter of fact.
A solace for those supporting friends and family with dissociative pathology is knowing there are places and people who can help. It's about giving them the tools and knowledge they need to be effective allies in the healing process. This support system is truly valuable for everyone involved, you see.
Addressing Misconceptions
One of the things Jules might encounter, and certainly what their loved ones might learn, is how many misconceptions there are about DID. The "My text" notes that it's often misunderstood and portrayed incorrectly. A hospital stay can be a time to clear up these wrong ideas, you know.
For example, some people think DID means a person is violent or dangerous. This is simply not true. Most people with DID are not violent, and if anything, they are more likely to be victims themselves. This is a very common and harmful misconception, so it needs to be addressed.
Another common idea is that DID is rare, or even fake. While it is a rare condition, it is absolutely real. It is recognized by major mental health organizations. Dispelling these myths is a vital part of helping someone with DID feel accepted and understood, you know.
A man with dissociative identity disorder wrote about 13 misconceptions he's heard about his condition. These often include ideas that alters are always obvious, or that therapy aims to "get rid" of alters. In truth, alters may not always be noticeable, and therapy often focuses on cooperation and integration, not elimination, you see.
The hospital environment provides a safe space to talk about these stigmatized views. It helps Jules, and others, feel less alone in facing public misunderstanding. It's about replacing false ideas with accurate information, which is a pretty big step toward healing, you know.
Learning the truth about DID can be empowering. It helps individuals and their families advocate for themselves and educate others. This knowledge helps to chip away at the stigma that often surrounds mental health conditions, and that's a very good thing.
Life After the Hospital
Leaving the mental hospital is not the end of the journey for someone like Jules. It is more like a new beginning. The hospital stay provides a foundation, but continued support is very important for long-term well-being, as a matter of fact.
A discharge plan would be put in place. This plan includes arrangements for ongoing talk therapy sessions, possibly with the same therapist or a new one who specializes in DID. It also covers any medications that might be helpful, though talk therapy is the primary treatment, you know.
Connecting with outpatient support groups or community mental health services is also a big part of this plan. These connections help Jules maintain the progress they made in the hospital and continue to build a supportive network outside. It's about staying connected and getting help when needed, you see.
The goal is to help Jules live a full and meaningful life, managing their condition with the skills they have learned. It's about continuing to work towards internal harmony and stability, so they can thrive in their everyday world. This ongoing process is pretty important for lasting change.
It is a path of continued growth and self-discovery. The tools and insights gained during the hospital stay are meant to be used and built upon. This allows Jules to keep moving forward, even when challenges come up. It's a journey that keeps unfolding, naturally.
The support system created both inside and outside the hospital plays a crucial part in this ongoing process. It provides a safety net and encouragement for Jules as they step back into their regular life. This continued care is a very important piece of the puzzle, you know, for long-term success.
Frequently Asked Questions
What is the most common cause of dissociative identity disorder?
While the "My text" doesn't specifically list causes, it's generally understood that DID often develops as a way to cope with severe, repeated trauma during childhood. This trauma is usually extreme and ongoing, like abuse, and it happens at a time when a child's personality is still developing, you see.
Can dissociative identity disorder be cured completely?
The term "cure" is not always used for DID. Instead, the goal of treatment is to help the different identity states integrate or learn to work together. This can lead to a significant reduction in symptoms and a more unified sense of self, allowing the person to live a much more stable and fulfilling life, you know. It's about managing and healing, rather than erasing the past.
How long does someone stay in a mental hospital for DID?
The length of a stay can vary a lot, depending on the person's needs and the severity of their symptoms. Some stays might be shorter, for stabilization, while others could be longer for more intensive therapy. It's really about what each individual needs to get to a safer, more stable place, as a matter of fact.
Finding Peace and Progress
So, what did Jules do in the mental hospital? They would have engaged in intensive talk therapy, the primary treatment for DID. They would have learned new coping skills, participated in group support, and started to address the many misconceptions surrounding their condition. It's a process of deep personal work, you know, aimed at bringing about a sense of internal peace and integration.
For anyone experiencing dissociative symptoms, or for those supporting a loved one, knowing that help is available can make a big difference. The journey toward healing from dissociative identity disorder is a personal one, but it is not one that has to be walked alone. There are resources and people who genuinely care about helping others find their way to a more whole and peaceful existence.
If you or someone you know is struggling with symptoms of dissociative identity disorder, reaching out for professional help is a very important first step. You can learn more about mental health support on our site, and find resources to help yourself or a loved one by visiting our dedicated support page. Remember, understanding and support are key to moving forward, especially today, on this day, April 24, 2024.
Dissociative Identity Disorder (DID): Symptoms, Causes, & Treatments

DO DOES DID DONE | Basic english grammar book, Study english language

Cómo Usar el Verbo Auxiliar DID - YouTube